Experiencing social anxiety in the midst of managing a chronic health condition can pose many challenges, particularly regarding developing and maintaining a strong social support system.
Feelings of doubt and insecurity regarding one’s sense of belonging, acceptability and freedom to know and be known by others are often core features underlying social anxiety. These feelings and beliefs give rise to apprehension and worry regarding being judged negatively by others, and can unintentionally lead to unhelpful habits of coping such as avoiding situations, perfectionism, or people-pleasing.
A chronic health condition is understood as a condition that requires medical attention and/or restricts a person’s daily life and lasts at least one year. The most common of these in the United States include but are not limited to heart disease, stroke, diabetes, and cancer. Out of all the health conditions in the United States, chronic illnesses/diseases are the most prevalent, costly, and responsible for seven out of ten deaths in the United States (ADAA, 2023).
For those who struggle with social anxiety in addition to the challenge of a chronic health condition, the intensity of these feelings can become easily overwhelming in the midst of the multiple health and life stressors they may be facing. In fact, such elements of social anxiety may often be missed or brushed aside in the face of other demands. In some cases, elements of an illness or aspects of treatment may lead to changes in mood, energy, or physical appearance which can themselves silently contribute to the development of social anxiety.
Like an invisible constraint, if unaddressed the impact of social anxiety can limit one’s development of needed social support. Furthermore, it can make difficult adhering to and getting the most out of many aspects of appointments with doctors and other aspects of care.
Engaging Support Isn’t Always Easy!

Many people with chronic health conditions are advised of the benefits of social support and encouraged to reach out in ways such as joining a support group, being open with friends and family about what’s going on, or initiating services with various providers. However, the anxious automatic thoughts and predictions common in social anxiety can make it very difficult to initiate and follow through with many of these sound ideas. For example, thoughts might arise such as:
“I’ll look weird or awkward.”
“I won’t know what to say.”
“Others will judge me or think I’m flawed for having my illness.”
“I’ll burden others.”
“I’ll be forced to talk about my illness again and again.”
“I’ll be seen as weak.”
Such automatic predictions lead to apprehension and all too often the short-term way to find relief from feeling anxious; by avoiding the situation. Falling into such a pattern of anxiety and avoidance can become a troubling barrier to developing rewarding connection, finding needed support in ways that work for you, and creating opportunities to experiment with and shift unhelpful thought patterns.
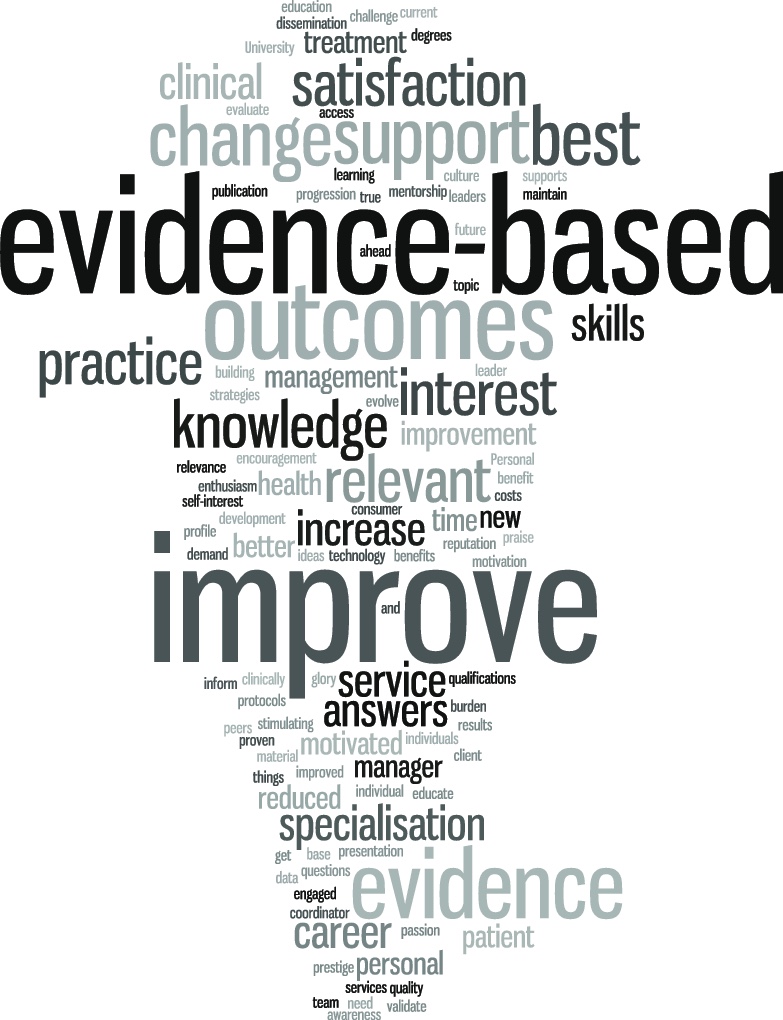
If you notice thoughts or images such as those listed above that come up and get in the way of connecting with others, it can be an opportunity to pause and practice shifting your response to these thoughts. In cognitive-behavioral therapy (CBT), one way we practice this is through cognitive restructuring, which can help you develop the skill of evaluating and shifting your automatic thoughts in more effective directions. Additionally, recognizing the moment of fear or shame attached to these thoughts can be a cue to move to a practice of self-compassion. Creating space for and recognition of the difficulty of these feelings, and moving your perspective to look at the bigger picture and what actions will take you towards growth and connection can be an empowering response to old sticky thought patterns.
Is it Self-Care or Avoidance?

Of course, when managing a chronic condition the practice of continuing to push oneself and tolerate through some discomfort needs to be balanced with the equal importance of when to say no to an opportunity and prioritize rest or self-care. Saying no might even be a therapeutic exposure challenge in and of itself, as it might require disappointing or disagreeing with someone else to act on your self-care needs.
It can often be very tricky to know the answer to the question of “When is something self-care versus avoidance?” The answer will likely vary situation to situation, though if one’s common anxious predictions and a jump in anxious feelings seem to be the driving force of wanting to say “no” to a social interaction, it is likely avoidance knocking on the door.
The examples above would be a perfect opportunity for a common strategy employed in CBT called behavioral experiments, further described in a video serious found here. Working with a trained CBT therapist to help identify negative thought patterns and predictions, and pinpoint ways to progressively experiment with and shift them in more adaptive directions can help push one through stuck points and develop more confidence and freedom in life.
The strategies introduced above can help you feel more comfortable and confident to engage, share, connect, set limits, and assert your needs: vital skills to help you discover and develop the support network that works for you.

Written by
Robert Yeilding, PsyD, A-CBT
NSAC – Bixby Knolls, Long Beach, CA
Director, YCBT Services
Sources:
Anxiety and Depression Association of America (2023): https://adaa.org/understanding-anxiety/chronic-illness-disease-anxiety-depression.